What is Prescript Assist?
Prescript Assist is a popular probiotic supplement that is marketed as following ancestral principles. The claim is that this product contains microorganisms found in soil, which are “natural” and what our ancestors consumed with their unwashed produce. Hence, the claim is that we’ve evolved with these microorganisms. Some of the other claims of this product are the following:
It (the formulation) can survive the harsh conditions of the gastrointestinal tract
It can permanantly colonize the gut
It has beneficial organisms in it
It has clinical evidence behind it
The product has prebiotics that will feed the bacteria in the product
Wow! The product seems like a miracle that addresses so many difficulties encountered by lactic-acid bacteria probiotics. The formulation has also changed in the past few years. The old Prescript Assist formula had 29 species of “soil-based organisms,” the new formula has 28, with several new species replacing old ones. Here are some of the microbes that are included in it:
Changes to the Prescript Assist Formula
| Old Formula | New Formula |
|---|---|
| Arthrobacter agilis | Arthobacter globiformis |
| Arthrobacter citreus | Azospirillum brasilense |
| Arthrobacter globiformis | Azosprillum lipoferum |
| Arthrobacter luteus | Azotobacter chroococcum |
| Arthrobacter simplex | Azotobacter paspali |
| Acinetobacter calcoaceticus | Azotobacter vinelandii |
| Azotobacter chroococcum | Bacillus amyloliquefaciens |
| Azotobacter paspali | Bacillus atrophaeus |
| Azospirillum brasiliense | Bacillus licheniformis |
| Azospirillum lipoferum | Bacillus megaterium |
| Bacillus brevis | Bacillus pumilus |
| Bacillus macerans | Bacillus subtilis |
| Bacillus pumilus | Bacillus thuringiensis |
| Bacillus polymyxa | Bacillus firmus |
| Bacillus subtilis | Brevibacillus brevis |
| Bacteroides lipolyticum | Cellulomonas fimi |
| Bacteriodes succinogene | Kurthia zopfii |
| Brevibacterium stationis | Micrococcus luteus |
| Kurthia zopfii | Nocardioides simplex |
| Myrothecium verrucaria | Pseudomonas fluorescens |
| Myrothecium verrucaria | Pseudomonas putida |
| Pseudomonas calcis | Rhodobacter sphaeroides |
| Pseudomonas dentrificans | Rhodococcus rhodochrous |
| Pseudomonas fluorescens | Rhodopseudomonas palustris |
| Pseudomonas glathei | Rhodospirillum rubrum |
| Phanerochaete chrysosporium | Streptomyces griseus |
| Streptomyces fradiae | Streptomyces griseoflavus |
| Streptomyces cellulosae | Streptomyces venezuelae |
| Streptomyces griseoflavus |
Let’s first explore whether it makes any sense to include these strains in a probiotic supplement. Some questions to consider:
Are these microorganisms found in the human gastrointestinal tract?
Are these microbes found in foods that humans regularly eat?
How do these microbes interact with each other?
How do these microbes interact with human microbes?
Will they produce antibiotics that could kill human bacteria?
What effects will they have on the immune system? Are they safe?
Have been they tested in large human studies, what about animal models?
Have they been tested over long periods of time?
What’s Actually Found in Prescript Assist?
Let’s do some investigative research. Searches of MEDLINE, the database of studies that are searchable using the search engine PubMed, yield almost no human or animal results for most of these microorganisms.
A lot of these organisms are used for agricultural and industrial purposes. Also, it’s interesting that several of the species found in Prescript Assist are not found in human or animal studies, but are found in this fertilizer product by Tainio Biologicals. Look at the italicized ingredients…
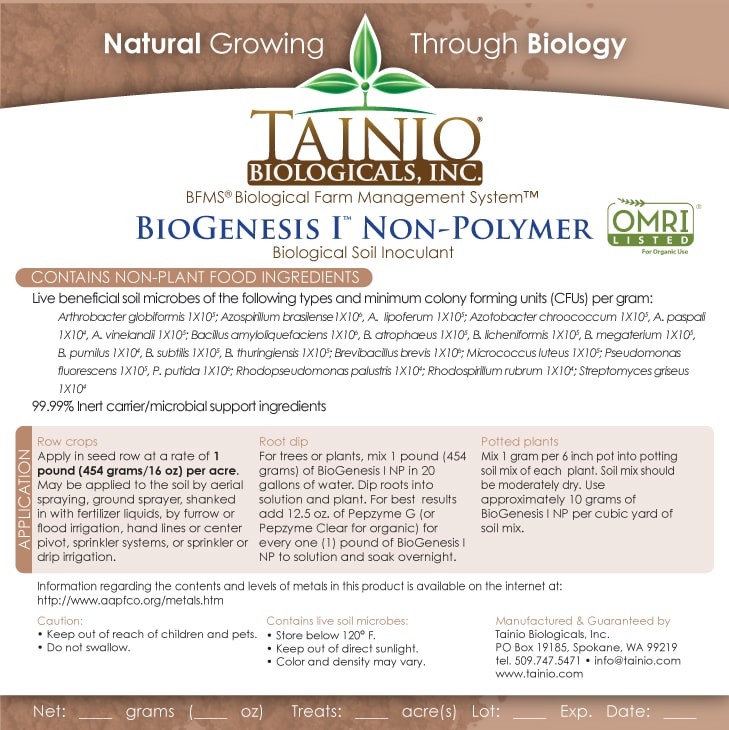
So Prescript Assist is literally repackaged soil fertilizer! A public legal blog also seems to support this with some uploaded documents
[Case 1:17-cv-00649-SS Document 57] “This discovery dispute arose when Enviromedica sought documents through a subpoena duces tecum from non-party Tainio Biologicals, Inc. (“Tainio”), an agricultural product supplier, who is Safer Medical’s sole source of key ingredients for a product at issue in this case. Dkt. #48 (Resp.) at 2. After Tainio produced documents on April 16, 2018, Defendants sent Enviromedica a Rule 26(b)(5)(B) “clawback letter” seeking to clawback six documents…”
[Case 1:17-cv-00649-SS Document 57] “Defendants (Safer Medical of Montana Inc.) do not dispute that they had an arms-length business relationship with Tainio [Biologicals] as their ingredient supplier.”
Also, several of the listed species above are known to produce antibiotics. One thing to consider is that if these organisms are spore-forming, antibiotic-producing bacteria, then it’s very possible that several of them (the clear majority in this product, which have not been studied) are competing with microorganisms in the gut for resources and may be difficult to control with antibiotics if they were to ever cause an infection.
The Clinical Evidence on Probiotics
The old formulation claims to be tested in a clinical trial and claims to be beneficial for symptoms of irritable bowel syndrome. In fact, most of the paleo community has promoted the product because of this clinical evidence. Let’s look at the study.
Here are the characteristics of this study:
A randomized trial with a placebo as a control
Double-blinded
Used a repeated-measures ANCOVA for data analysis (this increases the precision of the data)
Real limitations
Only two weeks long
Had 26 participants
Used an IBS questionnaire that is not validated
Poor reporting of the study
A randomized trial with 26 participants, that’s only two weeks long should not be used to market a product, and sadly there are numerous other limitations with this study. Many of these issues are discussed in this blog in depth. There is a reason drugs and many medical interventions must go through extensive testing before they’re allowed to be marketed as being effective for a condition/disease. Further, small sample sizes have lots of variability in the data and give imprecise results…
while larger studies or many studies can give a more accurate picture…
Graphics adopted from Micah Gallen’s & Ben Marwick.
And with something as complex as the microbiome, a two-week study does not justify the safety of this product. It’s also one study. No conclusions should ever be drawn from a single trial!
Despite this lack of evidence, several health gurus have been affiliates for this product and were hesitant to recommend the new formulation (when the product completely changed) because it didn’t have the “clinical evidence” to back it, however, there never was any good clinical evidence to back the product, even for the old formulation!
The Dirt on Probiotics
Various probiotic supplements have been studied for several conditions. Some of them have shown promise, most of them have not.
A note: If you’re going to ingest microorganisms to try to improve your health, you want to make sure that they’re safe and that they’ve been tested rigorously in human trials. If you’re going to be a bit more cutting edge because you’re desperate, you may at least want to be sure that the theory behind what you’re ingesting is sound.
For example, probiotics with lactic acid bacteria are found in fermented foods, like yogurt, which seem to be linked with improved digestive outcomes. They’ve been studied in in-vitro studies (petri dishes), in animal models, and in humans, and have been found to be relatively safe.
However, putting random organisms from the soil (a vast ecosystem, with who knows how many bacteria) doesn’t seem like a good idea. Especially when there’s no evidence to suggest these microorganisms will help.
I’d also suggest reading this interesting perspective about probiotic safety in the Journal of the American Medical Association.
According to Colleen Kelly, MD, a gastroenterologist and a professor at the Warren Alpert Medical School at Brown University, who was not involved with the research, the study is 1 of the first to show that some people’s guts resist probiotic colonization at the level of the intestinal lining, “where all the action is.”
The volunteers’ preexisting microbiomes largely determined whether they were permissive or resistant to probiotics. Interestingly, the fecal samples didn’t uncover these differences; both permissive and resistant participants shed comparable amounts of probiotic bugs, and more than the placebo group, in their stool.
To Elinav, the findings suggest that “our currently applied one-size-fits-all probiotic approach is probably incorrect.” Such interindividual variability means that some people may benefit from probiotics, while others may not.
This should come as no surprise, said Rob Knight, PhD, who directs the Center for Microbiome Innovation at the University of California, San Diego, and was not involved with the work. He pointed out that different people respond differently to the same foods, medications, and pathogens. “This is extending that to beneficial organisms,” he said of the study, adding that previous work has turned up the same variability.
There’s a general belief among some physicians and the public that consuming “good” bacteria in the form of a pill can edge out “bad” bugs and promote gut health even in healthy people. Yet in most clinical trials that involved healthy people, probiotics didn’t significantly change gut flora. With the Weizmann Institute study, the claim may be more dubious than ever, Kelly said: “The idea that people could just take probiotics for general health—you might be wasting your money.”
Help support the website!


